Wound Healing
Bacterial infection and wound healing in an ex vivo human skin model
Research by E. Pagès1, M. Pastore1, L. Rosselle2, A. Barras3, N. Skandrani2, A.R. Cantelmo4, R. Boukherroub3, P. Descargues1, S. Szunerits3
1Genoskin, 2TissueAegis, 3UMR8520 – IEMN, 4INSERM U1003
Scientific Context
Skin possesses excellent regeneration properties that allow its rapid healing upon dermal injury. If wounds fail to heal in an orderly and timely manner, chronic ulcers (e.g. diabetic foot ulcers, venous leg ulcers, pressure ulcers, etc.) develop. Efficient treatment of chronic wounds remains a global challenge. Next to wound debriding or hyperbaric oxygen therapy, a myriad of topical therapies and dressings are available to clinicians with very few having shown their effectiveness in promoting wound repair. Integrating nanomaterials into wound healing bandages is believed to be one possibility to overcome some of the current limitations. To test the potential of these innovative wound healing dressings, wound infection models are needed. Current research on wound infections is mainly conducted on animal models, which often limits direct transferability to humans and poses ethnic issues. Some of these limitations can be overcome by using an ex vivo skin model, WoundSkin®, human skin discarded from cosmetic surgery.
Wound Healing Processes Occurring in WoundSkin® Model
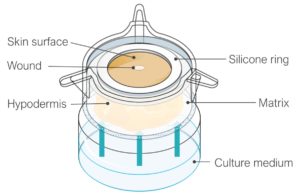
The skin explant, containing epidermis, dermis, and hypodermis, is embedded in a proprietary gel-like matrix with the epidermal surface left in direct contact with the air. To generate a wound, a defect of a controlled diameter is performed to remove all the epidermis and upper part of the dermis. A silicon ring is adhered to the skin surface to prevent lateral bacteria leakage. The system is mounted into cell culture inserts and maintained in standard cell culture conditions.
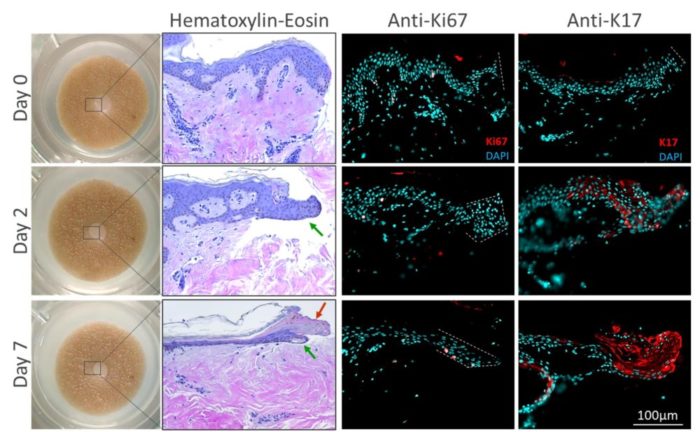
At day 0, the edge of the wound was a clear cut of the epidermis. From day 2, an epithelial tongue appeared and migrated until day 7. A crust was also visible at day 7. Cells in the migrating epithelial tongue were proliferating (Ki-67 positive staining) and expressing K17 which is a specific marker of keratinocytes migrating over the wound bed.
WoundSkin® recapitulates some aspects of wound healing
Please fill in the form below to access the full poster.
After submitting this form, you will receive an email with the link to access our poster.
Comments are closed.