Using NativeSkin® to evaluate poison ivy effects
A couple of months ago, Genoskin’s team started to wonder: “Why not try to better understand poison ivy dermatitis through our NativeSkin® model ?”
In this article, we summarize information about what is known regarding the poison ivy reaction and what happens on a macroscopic level when poison ivy toxin is applied to human skin.
What we know about poison ivy skin reaction
Allergic contact dermatitis (ACD) is a common skin condition resulting from cutaneous contact with an allergen. In the United States, the most common allergic contact dermatitis is caused by Toxicodendron species such as poison ivy, poison oak, and poison sumac. Approximately 50% to 75% of the US adult population is clinically sensitive to these species. However, poison ivy is the main culprit.

Legend 1: 3 different family of Toxicodendron are implicated in poison ivy-induced ACD
The major allergen responsible for Toxicodendron dermatitis is the urushiol, contained in the oleoresinous sap of the plant (3).
Let’s get technical!
Urushiol molecules consist of a catechol group substituted in carbon 3 by an alkyl group. The hydrocarbon chain is about 15 to 17 carbons atoms that can be saturated, polyunsaturated or unsaturated.
The exact chemical composition of urushiol may vary depending on the plant origin and other environmental factors. This is common all over the United States (4).
Elevated atmospheric carbon dioxide and warming temperatures have resulted in an increase in the biomass of poison ivy and related plants, widened their geographic distribution. This has also affected plant urushiol (3) content (increased) as well as its allergenicity (4) resulting in a larger number of cases every year.
The structural variations of urushiol can explain why we observe minor to extreme symptoms after skin contact. This is further compounded by the inter-individual differences in the human population.
Clinical characteristics of poison ivy-induced dermatitis
Contact with poison ivy plants results in clinical symptoms within 48 hours (4 to 96) (5).
While dermatitis can take up to 3 weeks to appear when first exposed to poison ivy, it can occur much faster after an initial sensitization.
Poison ivy-induced allergic contact dermatitis leads to painful and sometimes severe clinical manifestations (6). Itchiness, burning sensation, skin rashes, swelling and vesicles in extreme cases can last up to weeks in some individuals.
While symptoms are usually resistant to classic treatment such as antihistamines, high-doses of corticosteroids can be used in severe cases. Efficiency of this treatment is closely linked to timing (early after contact 3) and comes with side effects.
Toxicity pathway
Two types of mechanism of action can be observed after contact with poison ivy or one of the other Toxicodendron incriminated. Urushiol can act both as an irritant (7) and an allergen.
The most common is an allergic contact dermatitis which is a type IV hypersensitivity reaction. Urushiol can penetrate the skin within approximately an hour if not washed.
Catechols and alkyl side chains are immunologically inert on their own. However, when combined to form urushiol, they become immune sensitizers (5). Allergenicity will depend on the degree of unsaturation of the alkyl chain.
When urushiol catechols penetrate the skin, upon oxidation, they are converted into a quinine intermediate to become an hapten.
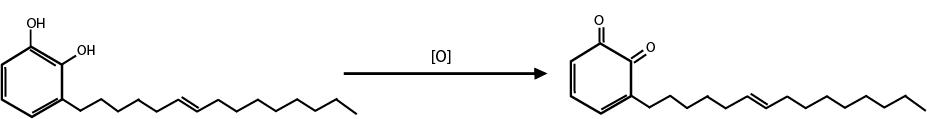
Legend 2: Urushiol mechanism of toxicity – Activation of urushiol upon oxidation of catechol group into a quinone group.
They bind with Langerhans cells (antigen-presenting cells) which lead to the activation of immune system mediators (8, 5).
T-cells are involved in the pathogenicity resulting in sensitization. Subsequent contact will produce a quicker reaction but the pathogenicity will also vary on the duration and the amount of exposure (5).
Interestingly, a study has shown that plant-derived lipid urushiol triggers CD1ɑ-dependent skin inflammation, driven by CD4+ T cells producing IL-17 and IL-22. This was performed in transgenic mice expressing CD1ɑ, a lipid-presenting molecule mostly expressed at the surface of Langerhans cells (2).
A second mechanism also known as the “black-spot poison ivy dermatitis” is less frequent as individuals often wash off the resin upon contact. But when urushiol isn’t washed off of the skin fast enough, one can observe black discoloration on the skin caused by the resin oxidation. The oxidized resin causes an acute irritant contact dermatitis (5) .
Poison ivy experiment on NativeSkin® model
Regardless of the above information, there is very little clinical data because of the lack of accurate characterized models (3).
In Genoskin’s lab in Salem, MA, we demonstrated the ability to reproduce the toxicity resulting in contact with urushiol as seen in Toxicodendron dermatitis. The ex vivo model developed can be used to further characterize human immune cells involved in the molecular pathological process underlying this allergic contact dermatitis. This is also an avenue to validate the efficacy of therapeutic approaches.
This is what we can observe during 3 days after treatment of the skin with synthetic urushiol. We will continue to develop novel experiments to further generate human data in our models and more results will come later in the spring.
References
- Gladman, Aaron C. “Toxicodendron Dermatitis: Poison Ivy, Oak, and Sumac.” Wilderness and environmental medecine, vol. 17, no. 2, 2006, pp. 120-128.
- Kim Y, Flamm A, ElSohly MA, Kaplan DH, Hage RJ Jr, Hamann CP, Marks JG Jr. Poison Ivy, Oak, and Sumac Dermatitis: What Is Known and What Is New? Dermatitis. 2019 May/Jun;30(3):183-190.
- Liu, Boyi, et al. “IL-33/ST2 signaling excites sensory neurons and mediates itch response in a mouse model of poison ivy contact allergy.” PNAS, 2016, https://doi.org/10.1073/pnas.1606608113.
- Yesul, Kim, et al. “Poison Ivy, Oak, and Sumac Dermatitis: What Is Known and What Is New?” Dermatitis, vol. 30, no. 3, 2019, pp. 183-190.
- Froberg, Blake, et al. “Plant Poisoning.” Emergency Medicine Clinics of North America, vol. 25, no. 2, 2007, pp. 375-433.
- Goodman, Rhonda, and Deborah Hollimon. “Allergic contact dermatitis : poison ivy.” https://www.medscape.com/viewarticle/730035_5.
- https://pubchem.ncbi.nlm.nih.gov/compound/Catechol
- Aptula, Aynur O., and David W. Roberts. Chemical Research in Toxicology, vol. 19, no. 8, 2006, pp. 1097-1105, https://doi.org/10.1021/tx0601004
Comments are closed.